Best Treatment For Fibroids, Uterine Fibroids(फाइब्रॉइड): Causes, Symptoms, & Treatment
Best treatment for fibroids, In this video SimpliHealth expert Gynaec Laparoscopic and Cancer Surgeon Dr. Heena Chawla will talk about Fibroids(फाइब्रॉइड) and its causes, symptoms, & treatment.
My friends and colleagues often call me regarding heavy bleeding. They have to change pads, menstrual cups, or tampons very frequently. So they are worried if they have फाइब्रॉइड. I would like to clarify that फाइब्रॉइडare not always the cause of heaving bleeding. But they are the most common reason why most females experience heavy bleeding.
- Is there any medical treatment for फाइब्रॉइड, or is surgery the only option?
- Does it cause problems in conceiving?
- Can it cause multiple abortions?
- Can it cause back and stomach aches?
Today we will be answering all these questions.
What is fibroids?/क्या है फाइब्रॉएड? | Best Treatment For Fibroids
Fibroids are simply tiny muscle knots, which are formed inside the uterus. More than half of the females are unaware that they have fibroids. फाइब्रॉइड can be detected in the ultrasound, which the patient does for other reasons. 70% of the females do not have any symptoms of फाइब्रॉइड. We have just detected fibroids in the ultrasound test. And the other 30% of the females experience symptoms like heavy bleeding, backache, or abdominal pain due to फाइब्रॉइड.
So, फाइब्रॉइड are muscle knots that arise in the uterus.
Fibroids Causes/फ़िब्रोइड कैसे होता है?
A lot of patients come to me and ask, what causes fibroids? There are various causes of fibroids, but science has not yet found a definite reason that we can pin the blame on.
- Hormonal imbalance: The imbalance of Estrogen and Progesterone hormones in the female can put her at risk of getting fibroids.
- Genetics: The risk increases if there is a history of फाइब्रॉइड in the family. That is, if the mother or elder sister have फाइब्रॉइड.
- Alcohol: Alcohol abuse can also put the female at the risk of getting फाइब्रॉइड.
- Obesity: It is found that females who are obese are at higher risk of getting फाइब्रॉइड.
- Menstruation: Females who start their periods at an early age are more likely to suffer from फाइब्रॉइड.
Fibroids Diagnosis
How are fibroids diagnosed? How does one know they have fibroids?
The first is, you go to the gynecologist, and he examines you and finds out you have fibroids. The second is ultrasounds. Like we said before, you detect fibroids in an ultrasound test. Once you have found out that you have fibroids, an MRI is suggested by the doctor for further investigation to determine the exact number, size, and locations of fibroids.
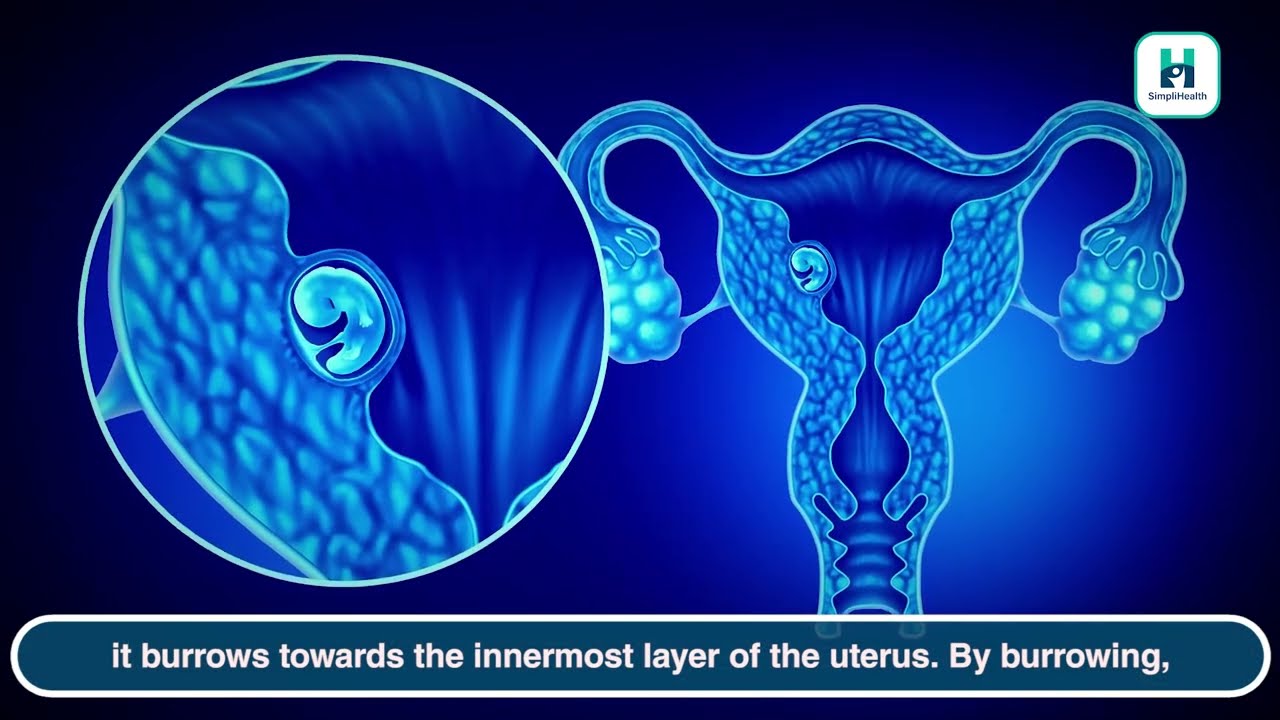
The uterus has three layers:
- Endometrium (inner layer)
- Myometrium (muscle layer)
- Serosa (serous layer)
The fibroid cyst can be in any of these layers. If it is in the innermost layer, then we call it submucosal fibroid. If it is the middle layer, it is called intramural. And if it is in the outermost layer, we call it subserosal fibroid.
Fibroids Symptoms
The symptoms of fibroids vary according to the location of the it.
Endometrium
The submucosal फाइब्रॉइड, situated in the innermost layer, causes the most symptoms like heavy bleeding, discharge, problems in conceiving, and recurrent abortion.
Myometrium
Moving on to the middle layer, the फाइब्रॉइड in the middle layer of the uterus cause fewer symptoms.
Serosa
The Subserosal फाइब्रॉइड is found on the outermost layer of the uterus. These are the least problem-causing fibroids. Even if they grow in size, they do not cause many troubling symptoms.
Till now, we’ve talked about heavy bleeding, but what are the other things that happen?
Backache and abdominal pain can occur. The fibroids grow in size up to 10, 12, 14, or even 16 cm and start putting pressure on the neighboring organs. So the patient starts showing pressure symptoms.
Front
If the fibroid is on the front side of the uterus, it will put pressure on the urinary bladder. This can cause symptoms like frequent urination.
Rear
If the fibroid is on the rear end of the uterus, it will put pressure on the rectum. This can cause constipation.
Fibroids of this size can cause pain or swelling that can go down to the legs; this is called radiating pain or swelling.
Fibroids Treatment/फाइब्रॉइड ट्रीटमेंट
We’ve talked about the symptoms; now, we will discuss the treatment for fibroids.
It is not necessary that the patient has to get surgery after the फाइब्रॉइड are detected in the ultrasound. Or it is also not necessary that we have to take medicines in all cases.
The treatment depends on the size, location, and number of fibroids, and whether the family is completed or they want to have more babies.. Based on all these things, a decision has to be made to choose the treatment method. Many patients come to us complaining about 2-3 cm big fibroids, with no symptoms, no heavy bleeding, no backache, no abdominal pain. Then, in this case, the patient needs neither medicine nor surgery. The patient is only put under observation. After a while, a scan is done to see how the fibroids are behaving.
Some of them just stay the same size and do not cause any problem. For fibroids this small, there is no need to worry. Some patients worry about these fibroids turning into cancer. However, fibroids are very simple benign knots. There is a less than 1% chance of fibroids turning into cancer. Every 1 in 5 women in India suffers from fibroids.
Now talking about the treatment of fibroids, there are 2-3 treatment options available for fibroids.
Medication | Best Treatment For Fibroids
Simple medication is stated for patients who experience heavy bleeding. These are non-hormonal medications. Besides, if we do not see any result with these medications, we start treating fibroids with hormonal medications.
There is a 21 days pack, estrogen, and progesterone combined pills or just progesterone pills. So we prescribe these to the patient to control the symptoms.
Other hormonal pills also help reduce the fibroids size. There are GnRH analogs or other hormones, but they cause side effects as they are stronger.
Hormone-coated Copper T
The second option for treating fibroids is hormone-coated Copper T. this is different from normal Copper T, as it is coated with hormones. This Copper T is inserted into the uterus and releases low doses of hormones. The advantage we have using this is that this action is only effective in the uterus, whereas the other hormone pills affect other parts of the body.
Using hormone-coated Copper T helps regulate periods, correct heavy bleeding, and improve the standard of living. And it also acts as a contraceptive. But it is not like we can use this for every patient. In cases where the fibroid is large or is putting a lot of pressure on the inner parts of the uterus, or the uterus has grown in size because of it, then we cannot use hormone-coated Copper T.
Surgery | Best Treatment For Fibroids
The third option of treatment is surgery. If the female has plans to start a family, and the fibroid is on the inner layer of the uterus, then it becomes very important to remove the fibroid surgically. This is because the baby needs a place to attach itself.
In females who do not plan to have a baby in the future, this treatment option is considered. There are two types in this. If the female wants a baby, then we only remove the fibroid. And in females who do not plan to have a baby, we remove the uterus itself with fibroids.
This surgery is done through laparoscopy. Even the big can be surgically removed by laparoscopy.
Bottom line
In the end, I would say you should consult a gynecologist. Discuss all the treatment options and then decide which medicine or surgery or hormone-coated Copper T would be best for you. Sit with your doctor and discuss if you need the surgery or not.
Discuss all this and make a decision. Thank you.